
Herniated Disc
- Degenerative Disc Disease
- Herniated Disc
- Lower Back Pain
- Neck Pain
- Sciatica (Lumbar Radiculopathy)
- Spinal Arthritis
- Spinal Deformities
- Spine Infections
- Spinal Stenosis
- Spine Trauma and Spinal Cord Injuries
- Spinal Tumors and Cancer
- Spondylosis
- Tingling in Arms (Cervical Radiculopathy)
- Upper Back Pain
Spinal discs play a crucial role in the lower back, serving as shock absorbers between the vertebrae, supporting the upper body, and allowing a wide range of movement in all directions.
What is a Herniated Disc?
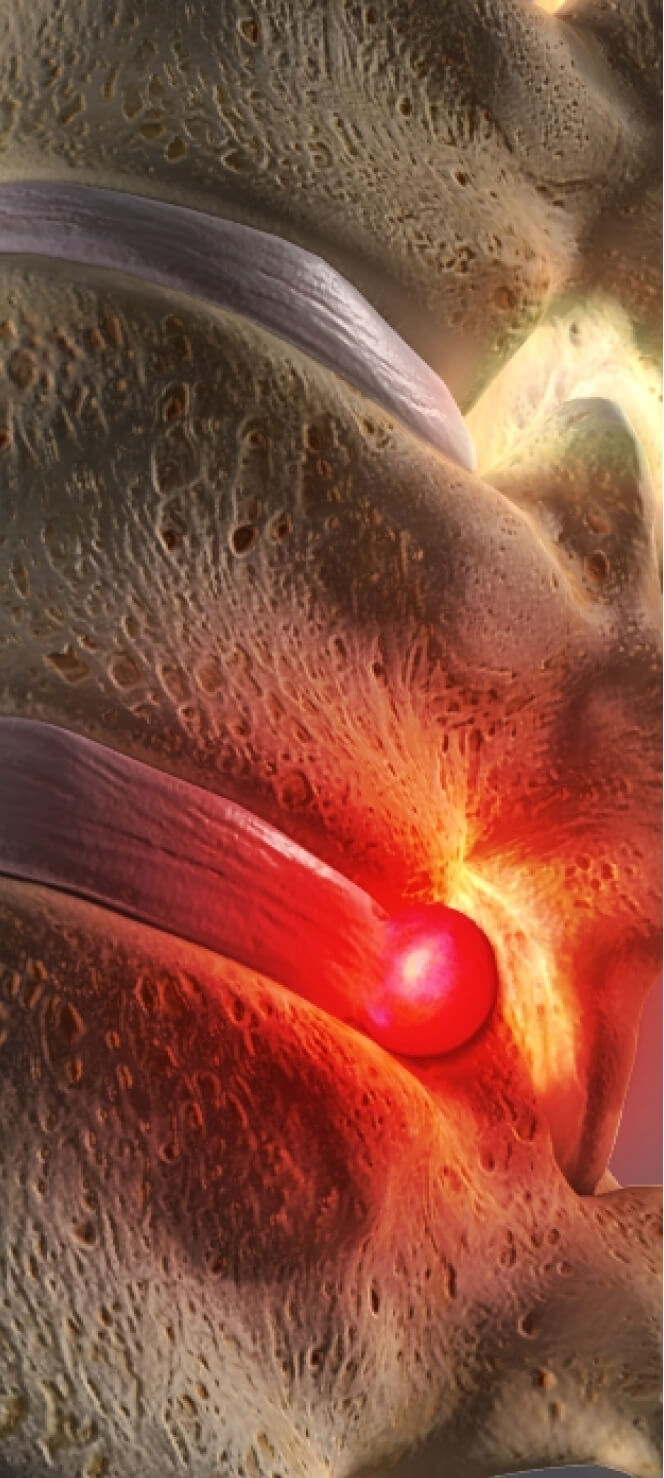
When a healthy disc in the spine degenerates, it can sometimes bulge or break open. It’s this abnormal rupture that is referred to as disc herniation, or herniated disc. While some people may experience pain, numbness or weakness due to irritated nerves, others have no symptoms at all. A clear medical diagnosis is the first step in understanding disc herniation and what can be done about it.
Herniated Disc
Between the vertebrae of your spine are soft discs. They let your spine twist and bend. They absorb shocks. But if damaged, the disc’s soft center can push through the disc wall. That’s a herniated disc. This bulge presses against nerves in your spine.
Herniated Disc (Cervical)
This condition is a rupture of one of the vertebral discs in your neck. A herniated disc can allow disc material to press harmfully against the spinal nerves.
What Causes a Herniated Disc?
In most cases, a herniated disc is the result of disc degeneration – gradual wear and tear associated with aging. In some cases, improperly lifting large, heavy objects can lead to a herniated disc. Less frequently, a herniated disc may be caused by a traumatic event, such as fall or a blow to the back.
Common Symptoms of a Herniated Disc
Not everyone suffers from symptoms–in fact, you can have a herniated disc without even knowing about it. While herniated discs can occur anywhere along the spine, the most common herniated discs occur in the lower back (lumbar spine). They can also occur in the neck (cervical spine) and, more rarely, in the upper back (thoracic spine).
The most common signs and symptoms of a herniated disc include:
- Arm or leg pain. The location of the herniated disc will determine the location of pain. A lower back herniated disc will cause pain in the buttocks, thigh and calf. A herniated disc in the neck will typically cause pain throughout the shoulder and arm.
- Numbness or tingling. A herniated disc often results in numbness or tingling in the areas where the nerves are irritated.
- Weakness. Weakness may occur in the muscles served by the affected nerves. You may experience stumbling, or inability to lift or hold items.
If you experience these symptoms longer than a week, or, if your pain becomes increasingly worse, call your doctor. Some symptoms require emergency medical attention. These include pain that inhibits you from performing daily activities, bladder or bowel dysfunction, and saddle anesthesia–the loss of sensation in areas of the body that would touch a saddle (inner thighs, back of legs and rectum).

Diagnosing a Herniated Disc
A medical, or “clinical” diagnosis focuses on determining the underlying cause of a patient’s back or neck pain. In order to reach a diagnosis, your doctor will go through a four-step process that includes a physical examination, a review of symptoms, a review of your medical history, and diagnostic tests.
1. Physical Examination
There are three main tests within a physical examination. The patient’s symptoms typically determine which one(s) will be performed.
- Nerve function in the legs and arms. This test involves tapping certain parts of the legs or arms with a reflex hammer to detect any abnormalities in the central or peripheral nervous system.
- Muscle strength. A neurological exam will be conducted to assess muscle strength. The doctor may also view the patient’s muscles to determine twitching or any other abnormal movements.
- Pain with palpation or motion. Palpating (touching) or moving certain areas can give the doctor some idea of where the pain is generating from.
2. Review of Specific Symptoms
Your doctor will review all of your symptoms. This includes where the pain is located, how searing or dull it is, and whether the pain feels better or worse based on certain activities, positions, or treatments.
3. Review of Medical History
A look into your medical background will help determine if there are any other possible contributors to your pain. Medical history includes information such as recurring health problems, family history of illness, previous diagnoses, past surgeries and treatments, and any other health concerns you may have.
4. Diagnostic Tests
If the doctor believes there is a disc problem, a diagnostic test may be ordered for confirmation and/or to gain additional information that may be helpful (i.e., location of herniated disc).
Diagnostic tests may include:
- CT Scan with Myelogram. A CT scan combines a series of X-ray images taken from different angles and uses computer processing to create cross-sectional, and very detailed images of structures inside your body. A myelogram consists of injecting a dye that can be seen on an x-ray into the sac around the nerve roots, which in turn lights up the nerve roots. Combining the CT and myelogram technologies provides the doctor with much better visibility of the nerves, including the nerve roots, during an exam for back pain.
- Magnetic Resonance Imaging (MRI). An MRI is a test that uses a magnetic field and pulses of radio wave energy to make pictures of organs and structures inside the body.
Treatment Options for Herniated Discs
Treatment options for a herniated disc vary depending on the severity of the symptoms. For some, no course of treatment is needed at all.
Non-Surgical Treatments for Herniated Discs
Conservative (non-surgical) treatment options include physical therapy, muscle-relaxant medications, pain medications, anti-inflammatory medications, and cortisone (epidural) injections. One or more of these, along with rest, moderate exercise, and avoidance of painful positions, is often enough to relieve people of their herniated disc symptoms. A process of trial and error is often necessary to find the right combination of treatment.
Minimally Invasive Surgery Options for Herniated Discs
If non-surgical treatments fail to provide relief within four to six weeks, surgery may be considered as an option. Many surgical procedures are minimally invasive (less cutting and entering the body), which result in smaller incisions, shorter hospital stays, less pain after surgery, and a faster recovery.
The most common surgery for a herniated disc is a discectomy. In this procedure, all or part of the damaged disc will be removed. Discectomy surgery is typically performed in two ways: as an anterior discectomy or as a laminectomy.
- Anterior Cervical Discectomy and Fusion: This procedure is for disc problems in the neck region. A small incision will be made through the front of the neck in order to reach the cervical spine. The damaged disc will be removed and replaced with a small plug of bone, which will eventually fuse the vertebrae.
- Spinal Laminectomy: This procedure will relieve pressure on the spinal cord. A part of the vertebra, called the lamina, will be removed so the disc and the nerves have more space.
In some cases, multiple spinal procedures are needed to reduce the pain. Other types of spinal surgeries include cervical corpectomy, laminoplasty, and spinal fusion. Since pain and symptoms vary from patient to patient, finding the right treatment can be complicated. However, working with one or more spine specialists, patients can find the best combination of treatment options for their pain.
If you are in the North Houston, Conroe, The Woodlands, Spring area and believe you need to see a spine specialist or have been recommended for minimally invasive surgery for herniated discs, call our office at 281-880-0700 to schedule an appointment with Dr. Fayaz.